Understanding Changes in Synapses May Provide Therapeutic Clues for Fragile X, Mouse Study Suggests
Written by |
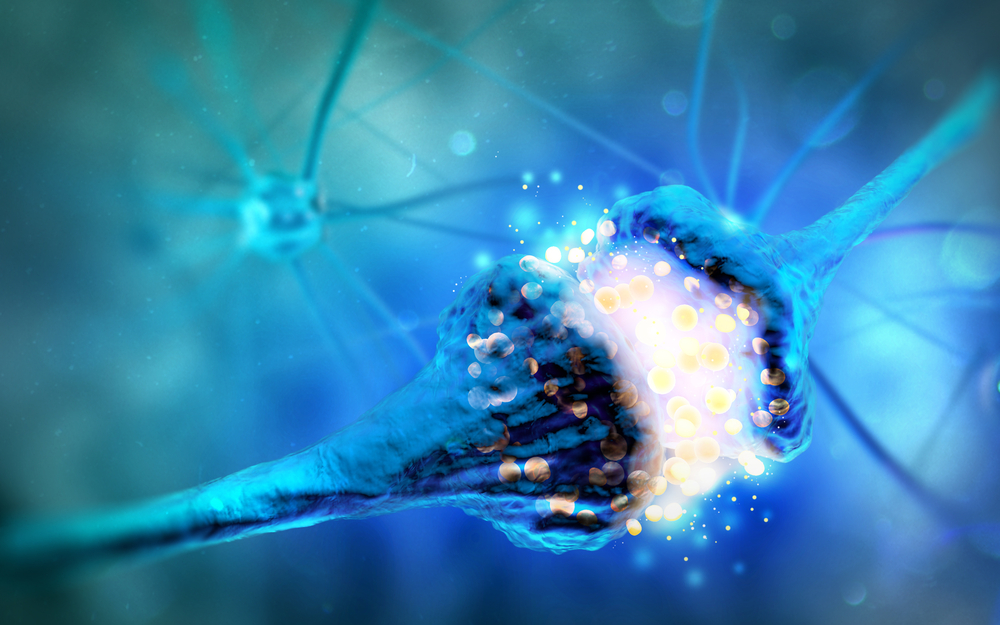
Scientists found evidence of a decoupling between structural and functional changes that weaken synapses (the place where nerve cells communicate). The findings may help identify new therapeutic targets and develop alternative therapies for people with fragile X syndrome, researchers said.
The study, “Dissociation of functional and structural plasticity of dendritic spines during NMDAR and mGluR-dependent long-term synaptic depression in wild-type and fragile X model mice,” was published in the journal Molecular Psychiatry.
Fragile X, the most frequent genetic cause of autism, is caused by mutations in the FMR1 gene, which provides instructions for making the FMRP protein. In normal conditions, FMRP controls the production of several other proteins at synapses.
However, in the absence of FMRP, protein production at synapses increases dramatically, resulting in synapse weakening and lack of synaptic plasticity (the ability to strengthen or weaken in response to information), which causes memory and learning impairments.
Until now, scientists generally accepted that changes in the function of synapses would be reflected in their outer structure, with weaker synapses having smaller spines — tiny structures in one of the communicating nerve cells — and stronger synapses having larger spines.
However, a group of researchers from the Picower Institute for Learning and Memory at the Massachusetts Institute of Technology (MIT) now have found evidence that challenges this assumption.
“We saw these breakdowns of correlation between structure and function,” Mark Bear, PhD, said in a press release. Bear is a professor in the Department of Brain and Cognitive Sciences at the Picower Institute and senior author of the study.
“One conclusion is you can’t use spine size as a proxy for synaptic strength — you can have weak synapses with big bulbous spines. We are not the only ones to make this case, but the new results in this study are very clear,” Bear said.
In their experiments, the investigators induced synapse weakening, also known as long-term depression (LTD), by activating two types of receptors — metabotropic glutamate receptor type 5 (mGluR5) and N-methyl-D-aspartate receptor (NMDAR) — in a mouse model of fragile X and healthy animals, used as controls.
After doing so, they found that even though activation of mGluR5 receptors caused synapses to become weaker, the spines did not shrink for at least one hour in either controls or mice engineered to mimic fragile X symptoms, indicating a decoupling between the two processes.
When they performed the same experiment while activating NMDAR, both processes occurred together in the two groups of animals.
When they interrupted the flow of ions (small electrically charged molecules) in NMDAR, the scientists found that synapse weakening was prevented, but spines still shrank.
To prevent spines from becoming smaller in healthy animals, they found that they had to either block the production of proteins at synapses directly, or indirectly by inhibiting a protein called mTORC1.
However, such strategy did not work in the mouse model of fragile X, indicating the existence of an unknown protein that induces spine shrinkage in these animals, to which Bear referred as “protein X.”
“The question is what is protein X,” Bear said. “The evidence is quite strong that there is a rapidly turned over protein X that is wreaking havoc in Fragile X. Now the hunt is on. We’ll be really excited to find it.”
“Further, our data indicate that metabotropic NMDAR signaling might be an interesting target of opportunity for development of novel therapeutics to correct synaptic pathophysiology [disease mechanisms] in fragile X,” the investigators wrote.