Tool Reactivates Gene in Stem Cells Harboring Fragile X Mutation, Study Shows
Written by |
Using a gene editing tool, researchers successfully reactivated the FMR1 gene — which is silenced in fragile X syndrome patients — in human stem cells.
The study, “Targeted reactivation of FMR1 transcription in fragile X syndrome embryonic stem cells” was published in Frontiers in Molecular Neuroscience.
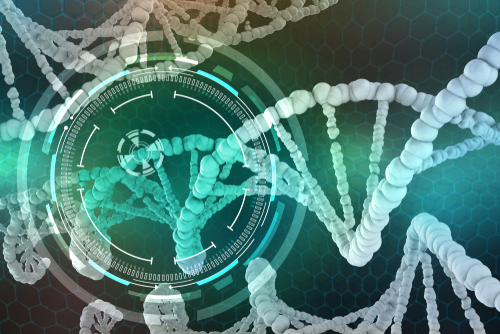
Fragile X syndrome (FXS) is caused by a mutation in the FMR1 gene that results from the addition of three extra nucleotides — the building blocks of DNA — to its sequence. This is called a CGG repeat, which varies in number from five to 55 in healthy individuals. The more repeats, the higher the risk of developing the disease.
This mutation results in the loss of the fragile X mental retardation protein (FMRP), the protein that is produced by the FMR1 gene.
Treatments tested so far attempt to compensate for the loss of the FMRP protein and usually target only one of the protein’s functions. However, they have proven insufficient to treat the disease.
Researchers believe one potential explanation for the lack of success in human clinical trials to date is that the different functions played by FMRP in nerve cells and other cell types may be difficult to correct with any treatment targeting only one dysregulated molecular pathway.
In this new therapeutic approach, researchers from the University of Michigan and the VA Ann Arbor Healthcare System used the CRISPR/Cas9 gene editing technology to target the CGG repeat that causes the mutation, and reactivates transcription of the silenced FMR1 gene.
Transcription is the first step required for protein production (DNA to RNA).
The CRISPR/Cas9 system is a genome editing tool that can edit parts of the genome by removing, adding, or altering sections of the DNA sequence. This allows researchers to modify bits of DNA in a very specific and precise manner.
The team first used healthy kidney cells (with a normal sized CGG repeat) to show that CRISPR/Cas9 could efficiently target the FMR1 gene and enhance the production of the FMRP protein by eight times.
Later, the scientists tested this approach in embryonic stem cells — a type of cell that has the capacity to differentiate into any tissue in the body — with an FMR1 mutation, this way recapitulating what happens in the nervous system of a person with fragile X syndrome during embryonic development.
CRISPR/Cas9 was able to increase the transcription levels, measured by the amount of mRNA, of the FMR1 gene in these cells.
However, this effect was not seen at the protein level, with no significant elevation in FMRP protein production.
Importantly, the team saw minimal off-target (or nonspecific) effects of the treatment in embryonic stem cells, raising concerns about the activation or repression of undesired genes.
“Given that less CGG DNA methylation, more FMR1 mRNA transcription and more FMRP production in even a subset of cells in [fragile X] patients all correlate with better clinical outcomes and differential responses to pharmacological agents, even modest successes targeting these proximal events … may elicit meaningful effects on clinical phenotypes,” researchers wrote.
“Thus, this proof-of-principle study provides additional hope that such approaches will eventually lead to effective therapeutics in patients with [fragile X] while also raising concerns related to the generalizability of the approach to all cases,” they concluded.