Derivatives of Alzheimer’s Disease Precursor May be Valuable Biomarkers of Disease Activity in Fragile X, Study Suggests
Derivatives of an Alzheimer’s disease precursor may be valuable biomarkers of disease activity in fragile X syndrome, according to a recent study.
The results of the study, “Peripheral Amyloid Precursor Protein Derivative Expression in Fragile X Syndrome,” were published in Frontiers in Integrative Neuroscience.
Fragile X syndrome (FXS), the most frequent single genetic cause of autism spectrum disorder (ASD), is caused by the expansion of CGG repeats in the fragile X mental retardation 1 (FMR1) gene, which provides instructions for making a protein called the fragile X mental retardation protein, or FMRP.
Although recent studies have shed new light on the molecular mechanisms underlying FXS, the lack of validated biomarkers of disease activity continues to halt the development of disease-modifying treatments for people living with FXS.
“Biomarkers linked to disease mechanisms may be useful in screening participants, evaluating patient responsiveness to treatment, and identifying subgroups that may best respond to a particular treatment. In recent years, there have been efforts to identify either a single or combination of molecular markers in FXS,” the researchers wrote.
The amyloid-beta precursor protein (APP) is normally produced by different types of nerve cells, and is responsible for the formation of neural circuits. APP is also the precursor of the amyloid-beta protein, which serves as a biomarker of Alzheimer’s because abnormally high levels of this protein in nerve cells have been found to be involved in the development of the neurodegenerative disease.
Previous studies have shown that FMRP directly affects the levels of APP in the blood of children with fragile X, suggesting that APP could also play a role in fragile X and possibly be used as a biomarker of disease activity.
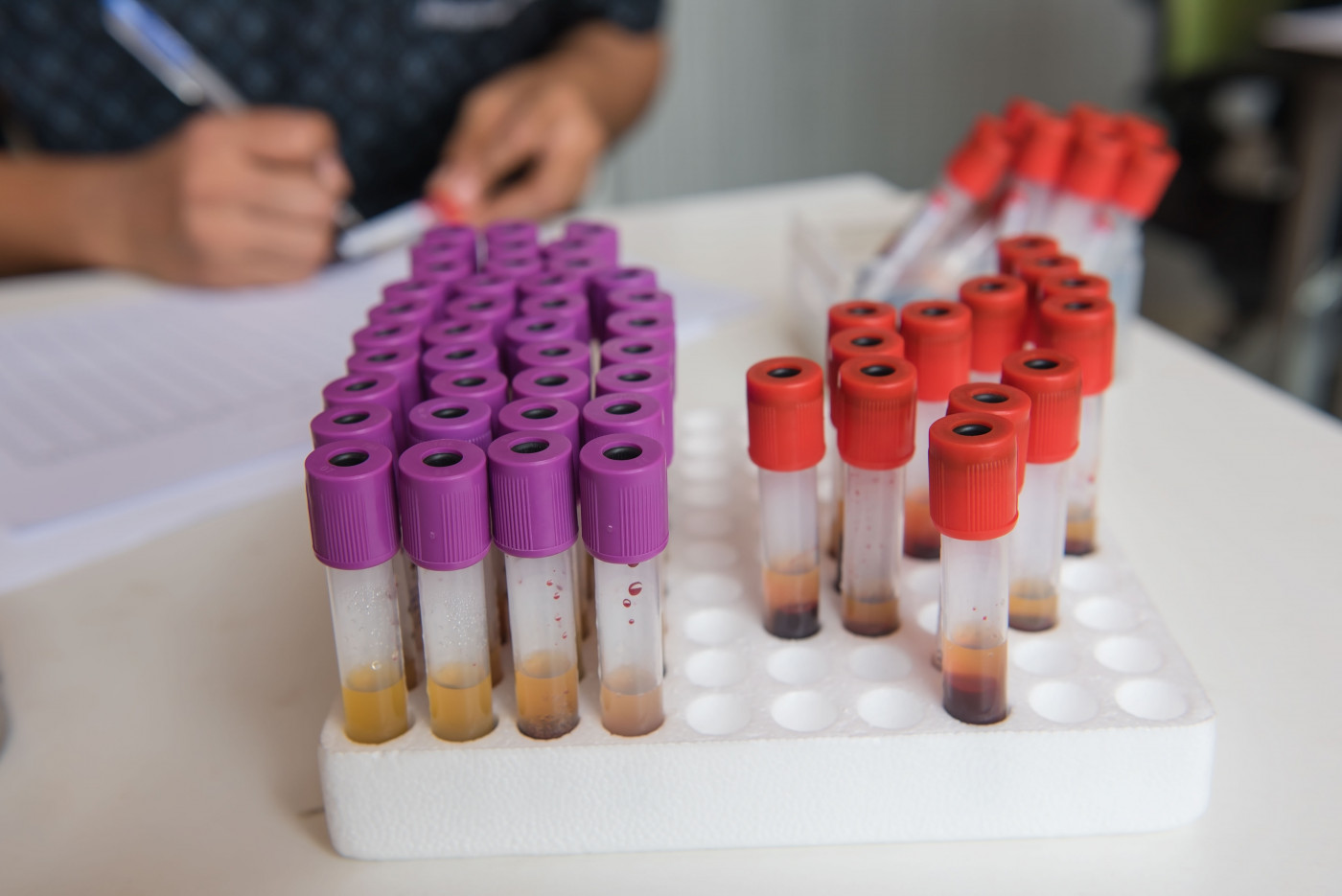
In this study, researchers from the Cincinnati Children’s Hospital Medical Center and their collaborators explored the usefulness of APP as a blood biomarker of FXS.
They gathered blood samples from 27 patients with FXS and 25 age- and sex-matched healthy individuals (controls). After collecting the samples, they isolated plasma — the liquid portion of blood that does not contain any blood cells — for analysis.
The levels of several APP metabolites — byproducts of APP metabolism (breakdown) — were measured in isolated plasma by Enzyme-Linked Immunosorbent Assay (ELISA), a technique that allows researchers to measure the amount of a specific protein of interest using an enzymatic reaction.
Analysis revealed the levels of two different forms of the amyloid-beta protein — amyloid-beta(1–40) and amyloid-beta(1–42) — were abnormally high in the plasma of patients with FXS compared with the controls. Of note, increasing research suggests amyloid-beta(1-42) accumulation in the brain as the event that triggers the Alzheimer’s-disease cascade.
Conversely, the levels of secreted amyloid precursor protein alpha (sAPPα), a metabolite that is thought to protect and support neurons in the brain, were much lower in patients with FXS than in healthy individuals.
However, no significant differences were found in the total levels of enzymes responsible for breaking down APP, suggesting the abnormal levels of certain metabolites in FXS patients were not directly linked to the total levels of APP-processing enzymes found in the blood.
Finally, the investigators also found the levels of most APP metabolites in the plasma tended to decrease with age in both FXS patients and healthy individuals.
“While we suggest that there is increased β-secretase [one of the enzymes that breaks down APP into amyloid-beta] activity in FXS, more work needs to be completed to determine the exact mechanisms leading to increased peripheral [amyloid-beta],” the researchers wrote.
“Still our findings provide new evidence of the promising potential of APP metabolite expression as a blood-based biomarker in FXS,” they added. “Ultimately, our work highlights the need for more thorough characterization of APP expression patterns with both behavioral and electrophysiological patterns in FXS, which may provide additional insight into the mechanistic roles of APP metabolites.”